Home | About OC | Continuing Education | Course Schedule | Registration | Accommodations | About Dr. Chan | Study Club | Doctor Education | Patient Education| Vision | Research Group | Science | Orthodontics | Laboratory | Dr. Chan’s Articles| GNM Dentistry | Contact Us | Partners | Dr. Chan’s Blogs
by Clayton A. Chan, D.D.S. – Founder/Director of Occlusion Connections, Las Vegas, NV
Within the field of dentistry there are certain criteria by which functional health can be monitored, measured and quantified to access a patient’s physiologic masticatory health and/or dysfunction (impairment) whether a patient’s dental system is stable or not. Physiologic standards of homeodynamics of the masticatory system which includes the teeth, all the muscles of mastication and the temporomandibular joints ) have been recognized within the dental community for the past 50 years and must no longer be ignored by the dental healthcare professional.
“No one notices when things go right.” This simple homily underlies the fact that 95% of the US healthcare economy is allocated for direct medical care, and only 5% is allocated to health improvement.1
As in the field of medicine there a certain standards that every medical doctor recognize and uses as standards in determining the health of a human being. Vital signs are measurements of the body’s most basic functions. The four main vital signs routinely monitored by medical professionals and health care providers include the following:
- Body temperature – The average normal body temperature is generally accepted as 98.6°F (37°C). Some studies have shown that the “normal” body temperature can have a wide range, from 97°F (36.1°C) to 99°F (37.2°C). A temperature over 100.4°F (38°C) most often means you have a fever caused by an infection or illness.
- Pulse rate – A normal resting heart rate for adults ranges from 60 to 100 beats a minute. Generally, a lower heart rate at rest implies more efficient heart function and better cardiovascular fitness. A well-trained athlete might have a normal resting heart rate closer to 40 beats a minute.
- Respiration rate (rate of breathing) – Respiratory rate: A person’s respiratory rate is the number of breaths you take per minute. The normal respiration rate for an adult at rest is 12 to 20 breaths per minute. A respiration rate under 12 or over 25 breaths per minute while resting is considered abnormal.
- Blood pressure (Blood pressure is not considered a vital sign, but is often measured along with the vital signs.) – More than 120 over 80 and less than 140 over 90 (120/80-140/90) is a normal blood pressure reading. A little higher than it should be or lower one should make healthy changes to your lifestyle.
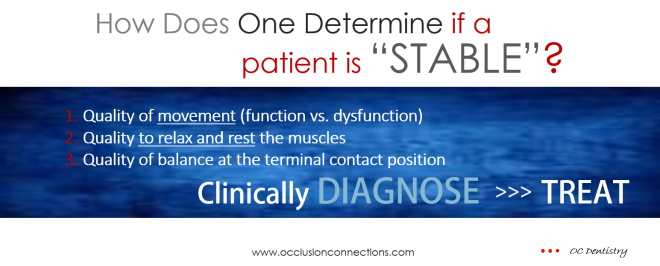
DETERMINING THE STABILITY OF A DENTAL PATIENT
Functional assessment tools exist, ranging from electromyography (EMG) which measures the activity in muscles in microvolts. Functional computerized mandibular scanning (jaw tracking/ CMS) accurately measures the motion and range of movement of the mandible in function in tenths of millimeters. Functional electrosonography (ESG) accurately measures and locates TM Joint sounds in function. It measures sound vibrational patterns in microV/division, amplitude, duration and frequency activity levels.
Consideration of the healthy state leads directly to an estimate of the functional capacity of the organisms stability. The recognition that there are optimal maximums vs. dyfunctional minimums is intrinsic to an effort to assess the amount of health an organism possesses. Health not only exists at the basal resting state but also exhibits substantial reserves. Such reserve relates clearly to the need for any organism to have a functioning ability levels to operate within normalized physiologic resting and functional parameters of health.
A multi-dimensional means of observing typical signature patterns, confirming hidden injuries, incorporates the clinicians expert skills, knowledge and training to visualize and conceptually grasp the functioning or dysfunctioning of body parts, organs, and neurovasomuscular systems while utilizing to the fullest extent the physical findings that form the clinical examination of each patient is key to assessing physiologic dental health.
Body Wellness and Masticatory Functional Health Must Meet PHYSIOLOGIC STANDARDS OF HEALTH
One must ask, “How are the muscles acting?” Are they acting normal healthy? or are the muscles acting pathologically strained (abnormal)? This is the subject that few professional within the dental healthcare system rarely acknowledge or focus on.
There are parameters (physiologic standards) for healthy masticatory system and there are parameters for dysfunction that can be objectively measured and quantified beyond the examining doctors subjective muscles palpation, visible range of jaw motion restrictions and or patient’s complaints.
The Following are the Dental Parameters (STANDARDS) of Masticatory Functional STABILITY.
- Muscle rest activity EMG levels – “Normal” EMG levels are 2.0mV +/- 5%. High EMG is not normal (pathologic, hyper active). Low EMG is also not normal (pathologic fatigued) – unhealth.
- Functional clench EMG (recruitment) activity levels – “Healthy” EMG amplitude is 200-250 mV +. Less than 150 mv is dysfunctional/impaired – unhealth.
- CNS EMG muscle balance before and after first tooth contact – Normal resting EMG levels with not fasiculation before clench and nor post synaptic responses immediately after clench. Normal occlusal balance is when temporal and masseter muscles activate to 5.5 mV simultaneously – balanced occlusion, healthy. If there is resting pre and post synaptic EMG responses before and after clench, this is unhealth to the central nervous system indication of unbalanced occlusion- dysfunction/impairment – unhealth.
- Functional terminal CMS velocity during open and close – 300 + mm/sec is excellent occlusion. 225 – 250 mm/sec. is unguarded occlusion. Poor occlusion is when terminal contact velocity speed is below 225 mm/sec. This is a clear indication of dysfunction/impairment – unhealth.
- Functional CMS swallowing pattern – Normal swallow shows teeth bracing against teeth. Abnormal swallow is when tongue braces between teeth, this is dysfunctional and an impaired restricted oral pharyngeal space/airway – unhealth.
- Functional CMS chew cycle at terminal contact – Normal healthy terminal contact should be sharp and detailed. Wide terminal contact indicates masticatory dyfunction and impairment – unhealth.
- Mandibular CMS range of motion – Normal maximum mouth opening ranges between 37-55 mm incisal edge to incisal edge. Normal left and right lateral jaw movements is 10-15 mm. Normal protrusive movement is 6-9 mm. Less than these parameters are considered limited or restricted jaw movements/dysfunction/impaired – unhealth.
- Functional ESG temporomandibular joint sound – No clicking, no popping, no crepitus sounds during jaw opening and closing is normal healthy. If joint sounds exists, that is not normal. Signature sound patterns greater than 0-400 filter on fast fourier spectral frequency analysis is indicative of degenerative joint degeneration (DJD). DJD is an indication that dysfunction and physical impairment – unhealth.
Special Note to All TMD Patients:
There are specific physiologic “objective” measured standards all TMD patients should have your treating dentist measure at the end of phase 1 orthotic treatment. These same measured tests should also be recorded at the end of phase 2 (finalizing treatment) to confirm your level of stability. These parameters have been recognized amongst clinicians within the dental profession. Those who are trained in the use and application of these technologies can be accountable and held to a higher standard. Just as in the medical healthcare field, a full panel of tests and blood work up is used to assess one’s level of health. So it is in the dental health care field. Objective data when recorded and interpreted correctly will help both the patient and the treating dentists whether their goals are being met.
Electromyography (surface EMG)
Physiologic resting status of a patients muscles can be measured and quantified using electromyography (surface EMG). They more specifically delineate and define hypertonic musculature in compromised patients. An EMG series differentially diagnoses between intra-capsular interferences (meniscal or otherwise) and extra-capsular interference (influence of the surrounding hypertonic muscular matrix) so as to determine the predominant dysfunctions. Defining the etiology of a patient’s predominant neuromuscular dysfunctions precluded misdirected diagnosis, recommendations and palliative treatment regimens.
Electromyography (EMG) utilizes eight channels monitoring the right and left posterior temporalis muscles, right and left anterior temporalis muscles, right and left massetters, and right and left anterior digastric muscles.
Functional Computerized Mandibular Scanning (CMS) – Jaw Tracking
Functional Computerized Mandibular Scanning utilizes Myotronics, K7, measuring vertical dimension, extent of lateral deviation upon opening and position where the deviation occurred, mandibular opening and closing movement and pattern during function from a frontal and a sagittal view, velocity of jaw motion from an incisal reference point during jaw opening and closing movements, and evenness or smoothness of jaw movement as opposed to jerking or uneven motion. This series is necessary to determine how the extra-capsular interferences of the surrounding hypertonic muscular matrix contributes to dysfunction.
Pathologic mal-occlusion, deficient intra oral vertical dimensions, restricted (limited) range of mandibular movements can be contributors to physical dental impairment/dysfunctions. Electro-diagnostic computerized jaw tracking patterns in a detailed manner help the dentist recognize poor mandibular function, guarded occlusal and terminal jaw closing patterns that result in bradykinesia (slow velocity movements) or dyskinetic (jerky jaw movement) disorders. Aberrant tongue swallowing patterns can impact cranio-facial growth and hinder the development of broad arch smiles and lead to narrow facial forms, deep and over closed bites as well as abnormal head and neck posture.
Functional Electrosonography (ESG)
Electrosonography (ESG) utilizes Myotronics K7 kineseograph which measures intracapsular TM Joint sounds against normalized data, duration of these sounds, exact location of the occurrence of these sounds during jaw opening/ closing, or lateral excursions, and a spectral frequency analysis of the sound. Without this information, one could not restore function free of intracapsular interference. This is more detailed and specific than subjective TMJ palpation.
Sonography measures intracapsular TMJoint sounds against normalized data, duration of these sounds, exact location of the occurrence of these sounds during jaw opening/ closing, or lateral excursions, and a spectral frequency analysis of the sound. Without this information, one could not restore function free of intracapsular interference, range of motion restrictions, and patient complaints.
Quiet functional moving temporomandibular joints should be the norm rather than abnormal clicks, pops and grating/crepitus sound patterns during electro-sonographic (ESG – joint sound) analysis.
References:
1. Iglehart JK. Influences on the health of population. Health Aff.2002; 21:7–8.
____________________________
To Read More: PHYSIOLOGIC REST – A Key to Effective Diagnosis and Treatment
- Stability: How Does Any Dentist Determine Joint, Occlusion and Muscle Stability?
- Relaxing Muscles with TENS
- TREATMENT
- DIAGNOSTICS
- Relating GNM Occlusal Treatment to the Diagnostic Craniomandibular Classifications
- Postural Alignment: Chan’s Dental Model
- What does Stable Mean – TMJ Lingo or Scientific Basis?
- The Lateral Pterygoid: Its Relevance in Clinical Dentistry
9061 West Post Road, Las Vegas, Nevada 89148 United States Telephone: (702) 271-2950
Leader in Gneuromuscular and Neuromuscular Dentistry